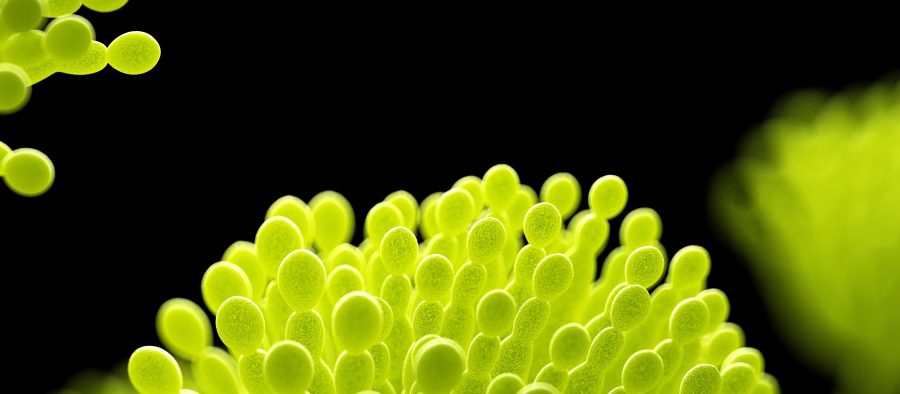
Self-report. Invasive pulmonary aspergillosis is a rare but serious pneumonia caused by the Aspergillus fungus. Infection is a known complication in patients with a weakened immune system, especially in relation to cytostatic therapy for acute leukemia or stem cell transplantation. Over the past decade, several retrospective reports have been published on invasive pulmonary aspergillosis associated with severe influenza infection, the so-called influenza-associated pulmonary aspergillosis (IAPA). [1]. The primary explanations are thought to be virus-induced damage to the airway epithelium with local lymphopenia, enabling invasive infection by Aspergillus.
In the largest study published to date, an incidence of IAPA of 19 percent was reported in 432 patients treated with Iva in the Netherlands and Belgium, most of whom lacked classic risk factors. [2]. Aspergillus infection is usually difficult to diagnose and usually requires bronchoscopy to perform fungal culture and detect Aspergillus antigen (galactomannan) in bronchoalveolar lavage fluid. In influenza patients, radiological findings are usually nonspecific, in contrast to immunocompromised patients where the most common finding is a typical dense, well-defined infiltrate with or without cavitation. Thus there is a high risk that IAPA will not be detected if the infection is not actively searched for. Effective treatment against Aspergillus exists and should be started immediately, as the infection is associated with a very high mortality rate.
Aspergillus is spread by inhaling its spores, so exposure depends on the climate and surrounding environment. Therefore the presence of IAPA in one country cannot be safely extrapolated to other countries. Because influenza patients in Sweden are not routinely tested for IAPA in EVA, information about its incidence is not yet available. We therefore conducted a prospective study on patients with PCR-confirmed influenza who were cared for in 12 Swedish ICUs during the four influenza seasons, 2019–2023. [3]. The IAPA classification is based on recently published criteria for distinguishing between invasive and colonizing diseases. The group included 55 patients. 42% were women, and the median age was 59 years (interquartile range 48–71). 5 patients (9 percent; 95 percent confidence interval 3.8-20.4 percent) were classified as probable IAPA, 4 of whom lacked classic risk factors. Bronchoscopy was performed in a total of 24 patients, all of whom were cared for on a ventilator, with IAPA findings in 12 percent of cases (5/42). Bronchoalveolar lavage fluid sampling was necessary to diagnose IAPA in all but one case. Mortality was significantly higher among patients with IAPA than among patients without IAPA (60 percent versus 8 percent; P = 0.01).
Our study is the first published prospective investigation of IAPA and confirms that it is also a problem in Sweden. IAPA typically occurs early in the course of care in Iva, and we therefore suggest that all ventilator-treated influenza patients be routinely tested for fungal infection and galactomannan in bronchoalveolar lavage fluid in relation to intubation. Rapid detection and treatment of these serious and potentially undiagnosed infections is important to improve the care of influenza patients at EVA Hospital.
Medical Journal 46-47/2023
Lakartidningen.se

“Extreme tv maven. Beer fanatic. Friendly bacon fan. Communicator. Wannabe travel expert.”






More Stories
How will artificial intelligence impact writing and the teaching of writing?
Spring's most popular topics – about barefoot people, GAPS, lymphatic system/self-care, thermal imaging, edibles in nature, medicinal mushrooms, etc.
Cervical cancer elimination project