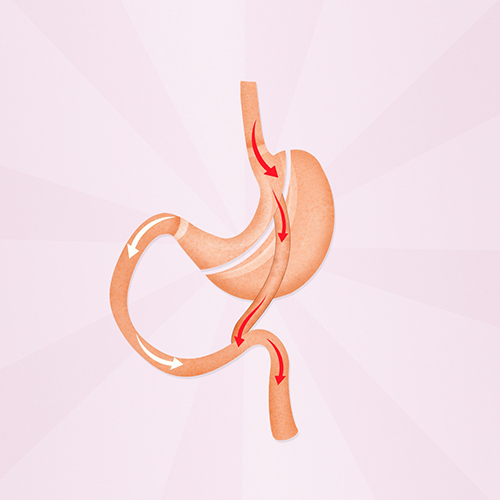
thesis. Today, obesity surgery is the most effective treatment against obesity and its consequences. The predominant surgical methods are gastric bypass and gastric sleeve. Between 2010 and 2015, the number of obesity surgeries in Sweden rose sharply, and we began to see more patients with late complications in the form of postprandial abdominal pain after gastric bypass. At the same time, gastric sleeve surgery was introduced as an alternative to gastric bypass.
In this thesis [1] Comparison of gastric sleeve and gastric bypass using BEST (Gastric Sleeve Bypass Trial), a multicenter randomized clinical trial based on registration in Sweden and Norway. [2]. The study included 1,735 patients in 23 hospitals. Patients were randomized to undergo surgery with either gastric sleeve or gastric bypass. Patients were included between 2015 and 2022, and perioperative data show that Scandinavian obesity surgery maintains a high level globally, with a low complication rate. No deaths were observed within 30 postoperative days, and there was no statistically significant difference in the complication rate: 1.7 percent serious complications (Clavien-Dindo ≥IIIb) in the gastric sleeve group and 2.7 percent in the gastric bypass group. The 5-year BEST results, with results for weight loss and complications, are expected to be presented in 2028.
To understand more about late complications after gastric bypass, with postprandial abdominal pain as the main symptom, a retrospective study was performed at Sahlgrenska University Hospital. We found that in many cases the symptoms were due to poor performance of the gastroenterostomy, and that some form of revision surgery for the gastroenterostomy resulted in improvement or freedom from symptoms in two-thirds of cases. To try to prevent these complications, changes in surgical technique have been proposed, including double stapling of the gastroenterostomy or a longer division of the mesentery between the gastroenterostomy and the gastroenterostomy in the primary surgery. The impact of these changes was highlighted in a registry study with data from the Scandinavian Obesity Surgery Registry and Patient Registry. We have been able to point out that surgical technical details seem to play a role, to the extent that double stapling is associated with a lower risk of early ileus, but by itself confers a slightly increased risk over time. On the other hand, if double stapling was combined with long mesenteric division, the risk of ileus was even lower in the long term.
In summary, we can conclude that the best study is off to a good start, with a low complication rate, and that gastroenterostomy is the Achilles' heel of gastric bypass. Furthermore, improved surgical technique to prevent complications in gastroenteral anastomosis, and revision surgery once complications occur, appear to be ways forward.
Medical Journal 7-8/2024
Lakartidningen.se

“Extreme tv maven. Beer fanatic. Friendly bacon fan. Communicator. Wannabe travel expert.”








More Stories
Why Rare Earth Metals for Electric Cars Are Crucial for Modern Mobility
“We want to promote critical rules approach”
“A lot happened during the trip,” Jönköping County Council